There are a lot of nurse practitioners in the US–over 400,000 (compared to around 900,000 MDs & DOs), and we are training 40,000 a year. But how they are going to be used is not entirely clear. Lynn Rapsilber is an NP whose organization, the National Nurse Practitioner Entrepreneur Network, is working to help her fellow NPs with their professional and business development. She came on THCB to discuss how NPs are developing and how she thinks NPs will contribute in the future as we deal with the current crisis in primary care–Matthew Holt
TytoCare–The Last Few Inches of Telehealth?
Tamir Gottfried, the Chief Commercial and Strategy Officer at TytoCare came on THCB to show us how their remote device works to deliver the last few inches of telehealth. Most telehealth is just a video call but with Tyto’s device, the patient can asynchronously (and/or synchronously) take their vital signs including videos and pictures of the skin, ears, mouth, heartbeat et al, and share it with their doctor. It actually amazes me that they haven’t been more popular but in the last few years Tyto has made significant inroads with health plans and providers delivering their devices, as well as adding chronic care management module, with a forthcoming smart clinic (AI) companion. Tamir explained who, how what and why to me, and gave a not too gruesome demo–Matthew Holt
Penguin–The Flightless Bird of Health AI
Fawad Butt and Missy Krasner started a new AI company which is building a big platform for both plans and providers in health care. Penguin Ai has a cute name, but is serious about trying to provide an underlying platform that is going enable agents across the enterprise. They are health care only, as opposed to the big LLMs. But does health care need a separate AI company? Are the big LLMs going to give up health? And what about that Epic company? Join us as we discuss how this AI thing is going to be deployed across health care, and how Penguin is going to play. Oh and they raised $30m series A to start getting it done–Matthew Holt
Boulder Care: Stephanie Strong & Marianna Zaslavsky
Stephanie Strong, CEO & Marianna Zaslavsky, the (relatively new) Head of Growth at Boulder Care came on THCB to tell Matthew Holt about their service which delivers medication assisted treatment for those suffering from substance used disorder, via telehealth. Stephanie has been one of the leading advocates for getting patients, especially those on Medicaid, access to treatment. She led a campaign to get the DEA to continue to allow substance abuse treatment using medication via telehealth. Marianna joined this summer with the goal of helping patients get access via managed care plans. We discussed a lot about the potential for Boulder to continue its harm reduction strategy for patients, and also the potential limits that might be coming via Medicaid reductions as part of the BBB. Stephanie & Boulder are supporting a campaign called Majority for Medicaid which is raising awareness about the impact of Medicaid cuts on these patients. Some of those stories are here
You can also text MAJORITY to 50409 to urge your representative to protect the promise of Medicaid.
New Bereavement Cost Calculator shows that grief is expensive

by EMMA PAYNE
Grief is expensive. In addition to the significant human impacts, research shows that bereavement leads to a 20%-30% increase in health care utilization.
Grief is also common. While we may not like to talk about it, 37% of Americans are grieving a recent death. The U.S. averaged 3.26 million deaths per year over the last five years and data suggests that an average of nine people grieve a single death. The CDC started measuring bereavement for the first time in 2021, but most health plans aren’t yet measuring the incidence or cost of grief.
So we decided to take a look. Here’s just some of what we found.
When a member is bereaved, health plans — especially those serving older adults — see significant jumps in utilization and costs across multiple claims categories. Examples include:
● 51% increase in Emergency Department visits and 43% increase in hospitalizations for bereaved spouses whose partners died in hospital
● 67% higher risk level for psychiatric hospitalization in the first year of bereavement for parents who have lost a child
● 74% of husbands and 67% of wives are hospitalized at least once in the nine years following the death of their spouse
● 463% higher odds of antidepressant use for people who have a prolonged grief disorder diagnosis
These increases lead to escalating claims costs that add up quickly, especially in populations 65+. But what are these costs? And what can insurers do to mitigate them?
To make these hidden costs visible, my team at Help Texts created a tool that health plans can use to model bereavement’s financial impacts. With just member numbers, the Bereavement Cost Calculator from Help Texts will estimate a health plan’s:
● Projected Per Member Per Month (PMPM) cost increase after bereavement
● Total cost impact of grief when no intervention is provided
● Estimated savings when plans provide Help Texts’ clinically sound, scalable, grief support for bereaved members
Consider a Medicare Advantage Plan with 250K members ages 65+. It should expect:
● Potential year one cost reduction (with intervention): $22.8M
● 11,500 members to be grieving the death of a partner or child
● 81,500 members to be grieving other losses (eg. parent, sibling, friend)
● Average PMPM increase (without intervention): $120
● Total estimated year one cost impact (without intervention): $134M *
What can a health plan do to save money and improve care and outcomes for its members? The numbers are powerful, showing that grief is expensive, but also that bereavement presents a clear opportunity to provide an impactful upstream intervention that can save millions, while also caring for people during what is often the loneliest time in their lives.
Help Texts is a clinically sound, scalable, bereavement intervention. With subscribers in 59 countries and all 50 states, Help Texts delivers affordable, multilingual grief support via text message. With extraordinary acceptability (95%) and 6-month retention (90%) rates, Help Texts’ light-weight solution makes it easy for health plans and others to improve health and community outcomes, while also realizing significant cost savings for those in their care.
Health Plans, particularly Medicare Advantage plans, can use the new bereavement cost calculator from Help Texts to estimate the true cost of bereavement and their cost savings when grief support is provided. The Bereavement Cost Calculator from Help Texts uncovers the savings potential when caring for grieving members. In less than a minute, you can start to see how much bereavement is costing, and how much could be saved by supporting members grieving the loss of a loved one.
Because the true cost of bereavement isn’t only emotional, it’s also financial. And for health plans, addressing both is the smartest investment you can make.
Emma Payne is the CEO of Help Texts
That’s More Like It

By KIM BELLARD
I’m always on the lookout for advances in healthcare that seem more like 22st century medicine than what we still experience in 2025. Way too much of it seems less advanced than we should be expecting in a world of AI, genetic engineering, nanobots, and the like. I often think of the scene in Star Trek IV where Dr. McCoy finds himself in a 20th century hospital and is appalled:
So I’m pleased to report on a couple of developments that seem like the future.
Transcranial ultrasound stimulation (aka “ultrasound helmet): You may not have ever heard of deep brain stimulation, unless you know someone who has advanced Parkinson’s, dystonia, essential tremors, or epilepsy. It turns out that electrical impulses to certain parts of the brain can help reduce the involuntary motions these conditions can result in.
The drawback is that deep brain stimulation is delivered by electrodes implanted deep in the brain. While this may not be quite as daunting as it sounds, people are still, you know, drilling holes in your head and pushing electrodes into your brain. You can imagine Dr. McCloy’s reaction.
Enter transcranial ultrasound stimulation. A new paper in Nature from researchers at University College London (UCL) and Oxford describes using a 256 element helmet to precisely aim ultrasound waves to accomplish the same results.
Our findings reveal this system’s potential to non-invasively modulate deep brain circuits with unprecedented precision and specificity, offering new avenues for studying brain function and developing targeted therapies for neurological and psychiatric disorders, with transformative potential for both research and clinical applications.
Professor Bradley Treeby, senior author of the study from UCL Medical Physics and Biomedical Engineering, said:
Clinically, this new technology could transform treatment of neurological and psychiatric disorders like Parkinson’s disease, depression, and essential tremor, offering unprecedented precision in targeting specific brain circuits that play key roles in these conditions.
The ability to precisely modulate deep brain structures without surgery represents a paradigm shift in neuroscience, offering a safe, reversible, and repeatable method for both understanding brain function and developing targeted therapies.
Continue reading…Telehealth safe harbor: a call to action for health plans

By AMI PAREKH
A little-noticed telehealth safe harbor provision tucked inside the One Big Beautiful Bill was a significant milestone in virtual care. Though it specifically addresses pre-deductible telehealth services in high-deductible health plans, the legislation has far wider implications for both care delivery and insurance design, especially in the commercial insurance market. In fact the permanent extension of a pandemic-era policy is a clear signal to health insurers that a new era of virtual care is under way.
The provision, which permanently extended an expired pandemic-era policy, is a win for employers and workers. After five years of uncertainty, employers are now empowered to provide telehealth services to their entire workforce at little or no cost, which has been shown to reduce access barriers and close gaps in care. For self-funded employers in particular, this flexibility in cost-sharing — combined with an increasingly sophisticated ecosystem of virtual care providers — will further accelerate innovation in benefits strategy and workforce well-being.
Less obviously, this employer-led innovation is also changing the virtual care landscape for a key partner: health plans. Though 20% of employers contract directly with specialized telehealth vendors, 78% rely on their health plan partners — and their vendors — to provide telehealth services for employees. As employers revisit their long-term virtual care strategy with new assurance in the wake of the safe harbor provision, health plans have an important seat at the table.
That seat is heating up, however. In a year when employer healthcare costs are projected to increase by more than 9%, employers are scrutinizing their partnerships and plan design to ensure that virtual care solutions are delivering meaningful value to their employees and their bottom line.
In a new annual survey from the Business Group on Health (BGH), more than three-quarters of employers said they are actively eliminating underutilized programs and underperforming vendors, or are considering doing so. Employers are also stepping up expectations in RFPs, evaluating potential healthcare partners on a growing list of factors and capabilities including performance guarantees, product and network design, reporting and analytics, and member experience.
In this light, the safe harbor provision is a call to action for health plans to evaluate their own virtual care strategy and partnerships through an employer’s lens. Three areas are especially important:
1. Quality
In the BGH survey, employers cited navigation to higher-quality providers and better quality transparency as top priorities — and virtual care is no exception. In last year’s survey, half of all employers expressed concerns about the quality of virtual care.
Continue reading…Labcorp, Blue Shield and my $34.95 co pay (part 5)
By MATTHEW HOLT
I have been on a quest to try to understand why I am being charged $34.95 by Labcorp for some lab tests that I think should be free under the ACA preventative care statutes, and for which my insurer Blue Shield of Californian has issued me an EOB with a $0 co-pay.
It’s been a microcosm of the chaos of American health care so far, If you want to catch up here’s part 1, part 2, part 3 and part 4
You may recall that I had paid a $50 co pay for the lab tests connected to my preventative annual wellness visit in 2024 (and I didn’t pay attention) but that when I got a $34.94 charge from Labcorp in 2025 and found that Blue Shield said my copay was $0, I decided to investigate.
I have had a lot of help from Rhea, a senior customer service rep at Labcorp who I think is having nearly as much fun with this as I am. She told me that the co-pay Labcorp tries to collect is the lower of $50 or whatever the total bill is. For the 5 tests I had, Labcorp’s agreed rate with Brown and Toland Physicians (the Blue Shield-owned IPA that contracts with their HMO, of which I am a member) was $34.94. So that is the answer as to that charge.
But it still doesnt answer a couple more questions.
- Why was a subsequent lab test I had as a follow up also shown by Blue Shield as a $0 copay on the EOB?
- Why weren’t the lab tests I had considered preventative under the ACA and therefore also free?
Rhea’s guess for the first answer is that Labcorp receives a capitated amount for lab tests from Blue Shield or Brown and Toland, and that the second test was somehow covered under that. Maybe, but then why wasn’t the first one?
The second question takes me further down a rabbit hole. Rhea dug out the order from One Medical to Labcorp. You can see below that the CPT codes are on it (what the tests actually are) and also what the related diagnosis codes are.
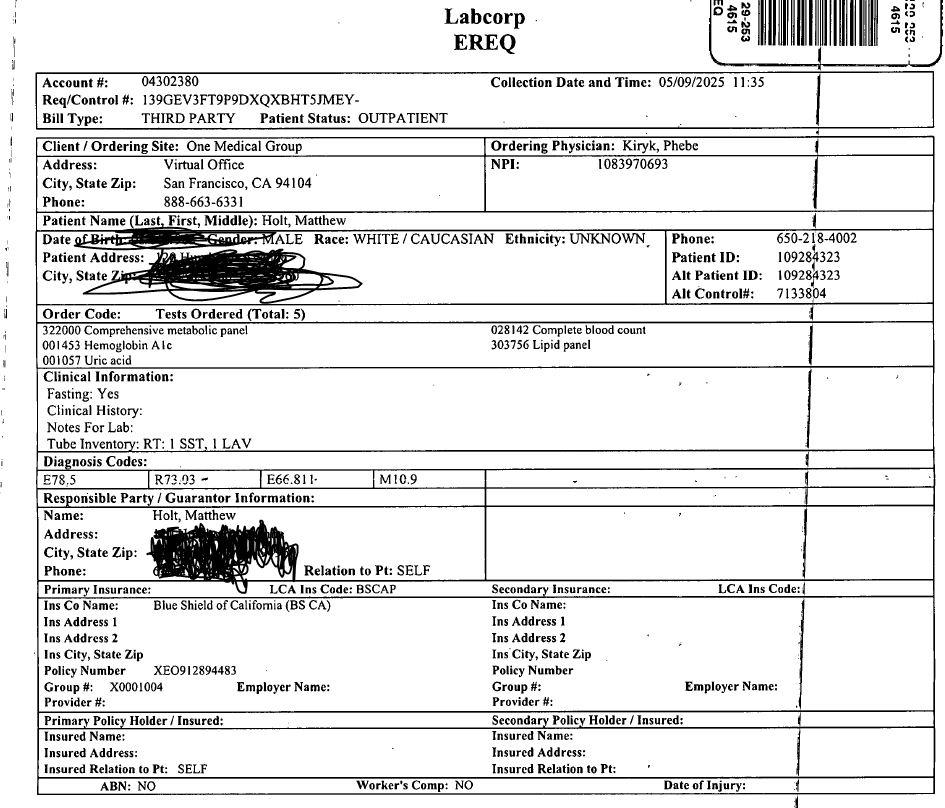
I of course asked chatGPT what those diagnosis codes were and the answer is
E78.5 = Hyperlipidemia (i.e. high cholesterol)
R73.03 = PreDiabetes
E66.811 = Obesity class 1
M10.9 = Gout
As you might suspect as a pretty typical 60+ year old American, I fit the bill for all those diagnoses. The CPT codes for the tests I had are complete blood count, Metabolic Panel, Hemoglobin (A1C), Lipid Panel, and Uric Acid (which causes gout).
Presumably all of those, with the possible exception of the Gout/Uric Acid, could be seen to be preventative. After all the CMS web site explains that preventative screening is free for “Annual Wellness Visits and Physical Exams, for instance with a primary care doctor and Health Screenings for blood pressure, cholesterol, blood sugar for diabetes, and various cancer screenings such as colonoscopies and mammograms”.
So why is this not free to me? Rhea from Labcorp suggests that Blue Shield initially issued me a $0 copay EOB but later should have reprocessed that when it got the bill from Labcorp, and told me to pay the $39.94. She also found that in addition to CMS suggesting what should be called preventative, Blue Shield of CA has a very long document with what it thinks is preventative care. You can see and download it here.
I asked ChatGPT to read it for me and after a bit of looking around we (that’s me and ChatGPT) concluded that E78.5 is in the list of applicable ICD-10 diagnoses codes for Annual health appraisal visits, which are a (free) covered service. So my high cholesterol should be screened for free.
On the other hand there’s a whole section on Page 28 of the document discussing pre-diabetes education but it doesn’t explicitly say that an A1C test is covered under the annual wellness visit. And if you go way down, to page 116, there’s a table that suggests that last year a Blue Shield review removed several of the diabetes codes, including R73.03.
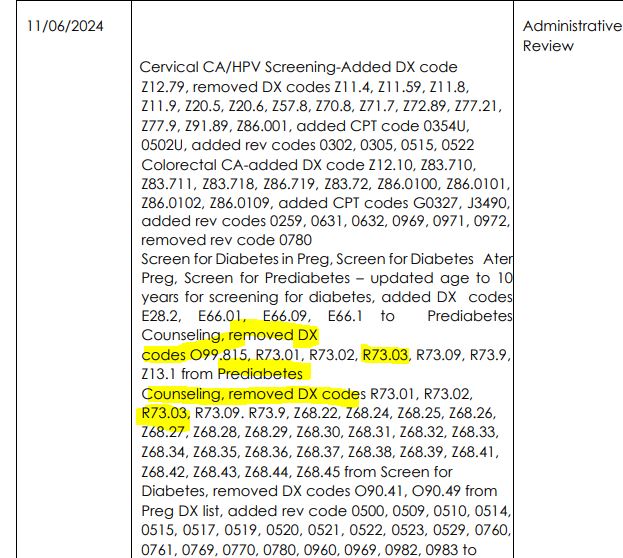
Now I am not going to pretend that I understand what the hell is going on in this document, and why (or whether) Blue Shield is able to change what CMS says it should do–if that is what in fact is happening. But it does seem weird.
And again, because there are no actual costs per test from Labcorp (there are charges per test but they are bundled and discounted on the bill), it’s impossible to tell what the contracted cost for each test was, and therefore whether I got some for free (as I think I should have) and what I was actually charged for.
Finally, I got very excited as Blue Shield sent me a message tonight which had an attachment which I think is a response to the grievance that was somehow filed for me by someone from their executive offices in part 2. But the attachment wasn’t properly formatted. So I don’t know what it says!
No less than I’d expect on this adventure.
But hopefully we are close to finding out who is charging whom for what and why!
UPDATE. I called Blue Shield’s grievance line and a nice customer service rep read me the letter that I couldn’t see online. Essentially Blue Shield has asked Brown and Toland to explain what happened. That grievance will take another 30 days! The rep wasn’t able to send it to me in my portal, but she could send me an email (It will be one of those secured ones that are super annoying to open). She told me it was sent while she was on the phone but 30 mins later, it’s not here!
Matthew Holt is the founder and publisher of THCB
Epic’s “Emmie” Chatbot Enhances the Patient Voice – For Their *Real* Customers

By MICHAEL MILLENSON
A Rock Health write-up of this year’s Epic Users Group Meeting captured the artificial intelligence vibe with a play on the names of three new AI chatbots rolled out by the country’s dominant electronic health record firm. “Epic Goes APE (Art, Penny and Emmie),” read the headline, using the first letters of the names of chatbots designed for, respectively, clinicians, revenue cycle managers and patients.
Emmie does positive things for patients – more on that in moment – but at its core the chatbot is a B2B play, designed to address the needs of the hospitals, medical groups and others whose fees have built the privately held EHR firm into an estimated $5 billion business.
Emmie is not an agent of patient autonomy. Its purpose is to help Epic customers (health systems and physician practices) provide more and better services to their customer, the patient, as long as that patient remains a customer.
That context is important. Yes, in a way it’s #PatientsUseAI, but that use is analogous to the AI algorithms deployed by Netflix. While you may marvel at their power of personalization, they’re never going to tell you that the best movie for your particular interest is harbored over at Hulu and, by the way, even if you’re watching tons of programs with medical themes, you’re still a couch potato.
I wasn’t present at the gathering at Epic’s Verona, Wisconsin headquarters, but news accounts and LinkedIn postings suggest that, unsurprisingly for this type of meeting, there was more drama than details. Much of what was unveiled and hinted at – the company said it’s working on more than 200 AI applications – will be rolled out over the course of 2026 and beyond.
Here’s Epic’s introduction of Emmie and Art from its LinkedIn account:
Informed by their chart and connected devices, Emmie is designed to support patients between visits. Whether it’s explaining test results in easy-to-understand terms, suggesting next steps, or guiding patients through open-ended conversations about their health, Emmie makes it easier for patients to stay on top of their health and walk into the exam room with a clear picture.
On the clinician side, Art is gathering data from Emmie to get the doctor the information they need before the visit even begins. Art is designed to reduce administrative burden, help doctors better understand their patients, and offer context-informed insights. This can take the form of generating pre-visit summaries, taking real-time notes, and even taking actions like placing orders or verifying prior authorization requirements.
That Rock Health analysis suggested that the real significance “may be less the function and more the channel,” since consumers are far more willing to share health data with their provider – in this case through Epic’s MyChart – than with a tech company (such as an AI vendor). “By capturing patient questions, decisions, and symptom-checking,” Rock Health noted, “Epic gains visibility into information consumers might hesitate to share with a generalist tech company. The EHR giant has already signaled that this data will feed back into [its] tools.”
Or as Epic did not say, “We empower our customers. We empower patients. We empower ourselves.” Good intentions alone do not get your product into use by more than half of all acute-care hospital beds in America, according to a KLAS estimate of market share.
At Healthcare IT Today, veteran tech journalist John Lynn sniffed out the actual schedule for all Emmie’s promised pro-patient wonders. According to Lynn (presumably from Epic itself),
- proactive outreach and images is coming in March, 2026
- active engagement in November, 2026
- future screenings arrive sometime in 2026 (no month given).
Bill payment, scheduling abilities using SMS (texting) and a voice agent are all “coming in the future.”
As I commented on the Epic LinkedIn post, “How about patient-reported outcome measures [e.g. Proteus Consortium’s], whether from an app linked to Epic (i.e., like Twistle by Health Catalyst or others) or the patient’s own wearables?” I tagged Seth Hain, Epic’s senior vice president of research and development, who played a prominent role at the meeting, but got no reply. (To be fair, maybe he took some vacation time after an intense few weeks.)
In a recent STAT First Opinion that took up the topic of autonomy, I asserted that true informed consent means physicians should be obligated to inform patients what Epic’s Cosmos system says about the likely outcomes of treatment for individuals with their clinical profile. Those predictions come from a database drawing on a mind-boggling 15.7 billion patient encounters. But patients should be able to access that information about different hospitals’ results on their own.
At the Users Group Meeting, Epic announced a further refinement of Cosmos, with founder and chief executive officer Judy Faulkner proudly announcing that the company will be able to “predict the future” for patients. (For a deep dive into Cosmos, I recommend the posts of veteran medical informatics expert Mark Braustein.)
Faulkner did what any smart businessperson would do. She spoke about how her company’s product would enable an important segment of customers, clinicians and health systems, to provide better care. What those customers actually do (or don’t do) for their “customer,” the patient, with the Epic software? Evidently “Not my job.”
Michael L. Millenson is president of Health Quality Advisors & a regular THCB Contributor. This first appeared in the “Patients use AI” Substack
Dr Kaelee Brockway on AI for physical therapy training
Dr Kaelee Brockway is a professor of education and physical therapy who has built a series of AI based “patients” for her PT students to train on. Kaelee is a pioneer in using these tools for training. She showed me the personas that she has built with LLMs that are now being used by her students to figure out how to train their soft skills–a huge part of any training. This a great demo and discussion about how clinical professionals are going to use LLMs in their training and their work–Matthew Holt










