In this episode of #HealthTechDeals, Jess is enjoying Cinqo de Mayo in an Addams Family-themed hotel where she is playing “the mummy” introducing health tech companies coming back from the dead. There’s gossip about Amazon’s pharmacy operation over supplying insulin, and there’s deals for Levels ($38m) in CGM analysis, Waltz Health ($35m) in pharmacy search, Safety Wing ($25m) for health insurance for nomads & Implicity ($23m) doing cardiac implantable monitoring in France.
#HealthTechDeals Episode 26: Hello Heart, Concert Health, Vivian Health, Curebase, Mendel.ai & Blue Spark
It’s the May the 4th be with you day! In Episode 26 of #HealthTechDeals, Jessica is huddling in Boston after the American Telehealth Association conference, and has Star Wars-related trivia. There’s gossip there, there’s more gossip about Cerebral & its ADHD med strategy. Meanwhile a lot of copy cats in deals today with Hello Heart ($70m) for hypertension, Concert Health ($40m) for mental health, Vivian Health ($60m) for nurse staffing, Curebase ($40m) for DCTs, Mendel.ai ($40m) for NLP & Blue Spark ($40m) for RPM — all joining very crowded markets.
Learning from This War

BY KIM BELLARD
There’s an old military adage that generals are always fighting the last war. It’s not that they haven’t learned any lessons, it’s more than they learned the wrong lessons. I fear we’re doing that with the COVID pandemic.
The next big health crisis may not come from another COVID variant; it may not be caused by coronavirus at all. Even if we learn lessons from this pandemic, those may not be lessons that will apply to the next big health crisis.
What started me thinking about this is a C4ISRNET interview with Mike Brown, the Director of the Defense Innovation Unit, and DARPA Director Dr. Stefanie Tompkins. Dr. Tompkins and Mr. Brown are both watching the war in the Ukraine closely. As Dr. Tompkins says in the interview, the war is a “really good test” about the programs her agency has invested in and/or is investing in for the future.
E.g., Russia has clear advantages in numerical superiority, and in “traditional” weapons like tanks, airplanes, ships, and artillery, but Ukraine has been able to blunt the invasion through asymmetrical warfare, using things that DARPA helped foster, including Javelin missiles, drones, satellite imagery, secure communications, and GPS. Even Russia’s vaunted cyber capabilities have been overmatched by Ukraine’s own capabilities. Current DARPA investments like hypersonic missiles and AI are being tested.
I’m comforted that DARPA and DIU are learning in real time what lessons their agencies can learn to help fight future wars, but I’m wondering who in our healthcare system, and who in our governments (federal/state/local), are not just fighting COVID but learning the bigger lessons from it to fight future crises.
I trust that smarter people than me are looking at this, but here are some the lessons I hope we’ve learned:
Information: it’s shocking, but we don’t really know how many people have had COVID. We don’t really know how many have it now. We like to think we know how many have been hospitalized and how many have died, but due to reporting inconsistencies those numbers are, at best, approximations.
We need early warning systems, like through wastewater monitoring. We need standardized public health reporting, with real-time data and a central repository in which it can be analyzed. We need easy-to-understand dashboards that both public officials and the public can access and base their decisions on. We can’t be building these during a health crisis.
Supply Chains: just-in-time, globally distributed supply chains are a marvel of modern life, bringing us greater variety of products at more affordable prices, but, in retrospect, we should have understood that in a global health crisis they would prove to be an Achilles heel. Masks and other PPE, ventilators, vaccines and other prescription drugs have all suffered from supply chain issues during the pandemic. Shortages led to unevenly distributed supplies and higher prices.
We’re never going back to the days of local production, but we do need to prioritize what things need to be produced regionally/nationally, how that production can scale in time of crisis, and how that production should be fairly allocated. The mechanisms to do that can’t be built on the fly.
The sick and the dead: Among the many images of the pandemic’s worst (so far) days, some of the most haunting are the ones of hospitals filled to overflowing, with patients on gurneys in hallways, or the refrigerator trucks filled with dead bodies. Our healthcare system’s capabilities for both were simply overwhelmed – as was the healthcare workforce.
Hospital beds are expensive to build, and expensive to maintain. We can’t afford a healthcare system that builds them for the worst case scenario. But we can learn from innovative efforts during the pandemic, like building temporary hospitals that can be expanded or contracted as needed.
Similarly, there has to be a strategy for dealing with dead bodies during a global health crisis, especially one in which those bodies themselves may carry ongoing risks. Existing morgues, mortuaries, and even graveyards may not be sufficient. There needs to be a plan.
Hardest to solve are healthcare workforce shortages. It’s not easy to train new healthcare workers, and retaining them when they’re stressed beyond belief proved to be a challenge. In a crisis, we need them all working at the top of the licenses, able to cross workplaces and even state lines, and properly supplied and compensated. None of those is a “normal” state of affairs for our healthcare system, and all are inexcusable in a crisis.
Telehealth: telehealth seemed to finally gets its day during the pandemic, with relaxed regulation, improved reimbursement, provider adoption, and consumer preference. It took pandemic to make us realize that making sick, potentially contagious, patients travel to get care is not a good idea.
That being said, now that the pandemic is in a more manageable phase, the bloom seems to be off the telehealth rose, with regulations being reapplied, providers not fully incorporating into their practice patterns, and patients returning to in-person visits.
Hey: it’s 2022. We have the technology to do telehealth “right.” Aside from, say, a heart attack or an auto accident, telehealth should always our first course of action. Our licensing, our reimbursements, and our work flows need to facilitate this – not just to prepare for the next health crisis, but simply as part of a 21st century healthcare system.
Communication: One of the most unexpected results of the pandemic is the distrust of public heath advice – vilifying public health officials, spurning mitigation efforts like masking or isolation, and spurring on the already-present anti-vaxx movement. “Science” is seen as in the eye of the beholder. It’s an information war, and health is losing.
We need the tools to fight the health information war more effectively. We need to learn how to communicate more effectively. We need to reestablish faith in science. We need responses to a health care crisis to be a health issue, not a political one.
————
We will be taken by surprise by the next health crisis. We had plans for a pandemic, but, when it hit, we fumbled every response. Next time we’ll be expecting another COVID, and, if it’s not, we’ll be caught flat-footed again.
The current crisis is, to use Dr. Tompkins’ words, a really good test for whether we’re working on the right things for our next health crisis. I’m not so sure we are.
Kim is a former emarketing exec at a major Blues plan, editor of the late & lamented Tincture.io, and now regular THCB contributor
#HealthTechDeals Episode 25: Biofourmis, Reify Health, Nex Health, and Amae Health
In this week’s episode of Health Tech Deals, everyone cheats on each other: Eugene Borukhovich is the guest host replacing Jess! Eugene is cheating on Jim Joyce, while I cheat on Jess; though Jess has cheated on me with Eugene before! Jess is on a cult retreat in Costa Rica, but Eugene and I have some deals to discuss: Biofourmis raises $300 million; Reify Health raises $220 million; Nex Health raises $125 million; and Amae Health raises “several million.”
-Matthew Holt
#HealthTechDeals Episode 24: Carbon Health, Clipboard Health, Source Health, and Diligent Robotics
Happy 4/20 everybody! Smoking weed live on Health Tech Deals is not to be encouraged, but Jess and I embrace the natural high of discussing the multitude of million-dollar deals in health technology: Carbon Health enters diabetes care; Clipboard Health raises $50 and $30 million; Source Health raises $3 million; and Diligent Robots raises $30 million.
-Matthew Holt
#HealthTechDeals Episode 23; Real, Iris Telehealth, 9am Health, Eko & Duos
In this episode of Health Tech Deals, Jess thinks the music has stopped as Rock Health reports Q1’s funding total being below Q4 2022! No $100m rounds today! But still $37m for Real; $40m for Iris Telehealth; only $16m for 9am Health but lots of Livongo connections; $30m for Eko and $15m for Papa-lookalike Duos
-Matthew Holt
#HealthTechDeals Episode 22: Viz.ai, PocketHealth, Eleanor Health, Recora, and Vytalize Health
3 big deals for this episode of Health Tech Deals! Tiger, General Catalyst, and e-Patient Dave are back! Check out this episode to hear my thoughts on them and on new deals in health tech: Viz.ai raises $100 million, PocketHealth raises $16 million, Eleanor Health raises $50 million, Recora raises $20 million, and Vytalize Health raises $50 million.
-Matthew Holt
DALL-E, Draw an AI Doctor
BY KIM BELLARD
I can’t believe I somehow missed when OpenAI introduced DALL-E in January 2021 – a neural network that could “generate images from text descriptions” — so I’m sure not going to miss now that OpenAI has unveiled DALL-E 2. As they describe it, “DALL-E 2 is a new AI system that can create realistic images and art from a description in natural language.” The name, by the way, is a playful combination of the animated robot WALL-E and the idiosyncratic artist Salvator Dali.
This is not your father’s AI. If you think it’s just about art, think again. If you think it doesn’t matter for healthcare, well, you’ve been warned.
Here are further descriptions of what OpenAI is claiming:
“DALL·E 2 can create original, realistic images and art from a text description. It can combine concepts, attributes, and styles.
DALL·E 2 can make realistic edits to existing images from a natural language caption. It can add and remove elements while taking shadows, reflections, and textures into account.
DALL·E 2 can take an image and create different variations of it inspired by the original.”
Here’s their video:
I’ll leave it to others to explain exactly how it does all that, aside from saying it uses a process called diffusion, “which starts with a pattern of random dots and gradually alters that pattern towards an image when it recognizes specific aspects of that image.” The end result is that, relative to DALL-E, DALL-E 2 “generates more realistic and accurate images with 4x greater resolution.”
Continue reading…Matthew’s health care tidbits: Hospital System Concentration is a Money Machine
Each week I’ve been adding a brief tidbits section to the THCB Reader, our weekly newsletter that summarizes the best of THCB that week (Sign up here!). Then I had the brainwave to add them to the blog. They’re short and usually not too sweet! –Matthew Holt
For today’s health care tidbits, there’s an old chestnut that I can’t seem to stay away from. I was triggered by three articles this week. Merril Goozner on GoozNews looked at the hospital building boom. Meanwhile perennial favorite Sutter Health and its price-making ability came up in a report showing that 11 of the 19 most expensive hospital markets were in N. Cal where it’s dominant. Finally the Gist newsletter pointed out that almost all the actual profits of the big health systems came from their investing activities rather than their operations.
None of this is any great surprise. Over the past three decades, the big hospital systems have become more concentrated in their markets. They’ve acquired smaller community hospitals and, more importantly, feeder systems of primary care doctors. Meanwhile they’ve cut deals with and acquired specialty practices. For more than two decades now, owned-physicians have been the loss leader and hospitals have made money on their high cost inpatient services, and increasingly on what used to be inpatient services which are now delivered in outpatient settings at essentially inpatient rates. Prices, though, have not fallen – as the HCCI report shows.
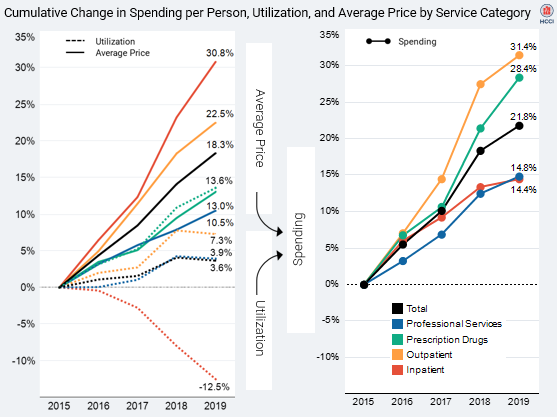
The overall cost of care, now more and more delivered in these increasingly oligopolistic health systems, continues to increase. Consequently so do overall insurance premiums, costs for self insured employers and employees, and out of pocket costs. And as a by-product, the reserves of those health systems, invested like and by hedge funds, are increasing–enabling them to buy more feeder systems.
Wendell Potter, former Cigna PR guy and now overall heath insurer critic, wrote a piece this week on how much bigger and more concentrated the health plans have become in the last decade. But the bigger story is the growth of hospital systems, and their cost and clout. Dave Chase likes to say that America has gone to war for less than what hospitals have done to the American economy. That may be a tad hyperbolic, but no one would rationally design a health care environment where non-profit hospitals are getting bigger and richer, and don’t seem to be able to restrain any aspect of their growth.
#HealthTechDeals Episode 21: IntelyCare, Avi Medical, Eleos Health, Evernow & Vivosense
Well at least my hair is under control today. What’s not under control is the chatter about Olive from Erin Brodwin at Axios, even if I don’t get Jess’ joke about the internet of Health Care. Meanwhile deals in nursing recruitment for IntelyCare ($115m), Avi Medical (50M Euros), Eleos Health ($20m), Evernow ($20m) and $25m for Vivosense–note my total inability to say their investor’s name!–Matthew Holt










