BY VINCE KURATIS, BRENDAN KEELER, and JODY RANCK
Recent regulations have mandated the use of HL7 FHIR APIs (application programming interfaces) to share health data. The regs apply to healthcare providers, payers, and technology developers who participate in federal programs. Many incumbent healthcare organizations are viewing these mandates as a compliance burden. That’s short-sighted. We recommend a more opportunistic POV.
APIs facilitate the sharing of health data across different devices and platforms. By adopting APIs, healthcare organizations can transform themselves from traditional service providers into powerful platforms that can connect patients, providers, and other stakeholders in new and innovative ways.
This blog post is the fourth in the series on The New Rules of Healthcare Platforms. In this essay, we explore the many benefits of API adoption for healthcare organizations and the key considerations that must be taken into account when implementing APIs:
- Healthcare’s Data Inflection Point
- APIs Enable Platform Business Models
- Barriers, Challenges, Reality Check
Healthcare’s Data Inflection Point
Compared to other industries, healthcare generates a disproportionately large amount of data. According to RBC Capital Markets, “30% of the world’s data volume is being generated by the healthcare industry. By 2025, the compound annual growth rate of data for healthcare will reach 36%. That’s 6% faster than manufacturing, 10% faster than financial services, and 11% faster than media & entertainment.”
Over the past 15 years, new regulations have driven digitization, data interoperability, and data sharing. The goal of regulations has been to liberate patient data that has previously been unstructured and trapped in patient silos. Venture capitalist Kahini Shah summarized these regulatory efforts in her article entitled Healthcare Data APIs – An Upcoming Multi-Billion Dollar Market?:
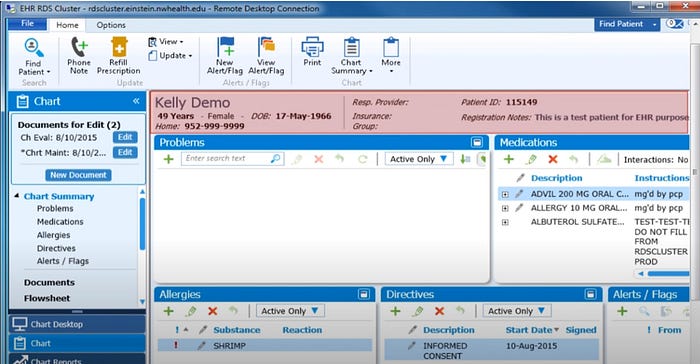
Recent regulation is forcing digitization, aggregation and transmission of medical records. Congress passed the HITECH Act in 2009, prompting the adoption of electronic health records. Before that medical records were paper based. Healthcare data is incredibly siloed, every American sees an average of 19 providers in their lifetime. Connecting these disparate electronic systems and having them exchange information is called interoperability. In 2020, the HHS and CMS implemented two rules that mandate patient access to their medical records and interoperability. These transformative rules give patients the right to access their data when they need and make it available via APIs. The interoperability rules state that there is no blocking – EHRs must allow data to be shared easily across different systems owned by different vendors.
Continue reading…