Greg Whisman is the Chief Medical Officer of CareMore Health, a venerable prepaid medical group caring for seniors. It’s been part of Anthem/Elevance for many years but this year spun off as part of a larger PE backed group called Millennium. We really got into the what and the how of primary care for seniors and, yes, we delved deep into the future of primary care. This is a topic that will never die on THCB and getting a real expert to opine on it was really valuable. This is a great conversation–Matthew Holt
Sami Inkinen, Virta Health
Virta Health is in the diabetes reversal business. It’s a medical group that for a decade has been aggressively coaching people with diabetes and cardiometabolic disease to radically change their eating habits–basically to eat the right things for them, to saity. Some how in a nation obsessed with processed food and carbs they have succeeded for a lot of people. And the business is growing fast, with over $160m in annual run rate. Ten years in since it started I spoke with CEO Sami Inkinen about how and why it works, and what the future for this approach is in a world of GLP1s (and no there’s no GLP sales in that revenue number!)–Matthew Holt
Concierge Care for all: What would it look like?

By MATTHEW HOLT
A few weeks back I wrote an article on what’s wrong with primary care and how we should fix it. The tl:dr version was to give every American a concierge primary care physician paid for by the government. We would give everyone a $2k voucher (on average, dependent on age, medical status, location, etc) and have an average panel of 600 people per PCP.
My argument was that a) this would be cheaper than health care now – due to cutting back on Emergency Department visits and inpatient admissions and that b) it would enable us to pay PCPs the same as specialists (roughly $500K a year). This would mean that many current ED docs, internists, hospitalists etc would convert to being PCPs. I also think that we could and would make better use of the now 400,000 nurse practitioners in the US. We would only need about 600,000 PCPs to make this work. Although it would double spending on primary care, it would reduce health care costs overall. (OK there’s some debate about this but the Milliman study linked above and common sense suggests it would save money).
There are obviously two huge issues with my proposal. First we would have to go through the conversion process. Second, we would have to do something big with the three major players who are sucking at the teat of health care $$ right now—those being big hospital systems and their associated specialists, health insurers, and pharma and device companies.
I don’t think that there will be any problem selling this to most doctors or to the American people.
The doctors know that they are trapped in the current system. This would free them to practice as they want to practice, and to remember why they got into medicine in the first place—to care for their patients holistically.
People know all too well that accessing primary care is both good for them and also very difficult. Wait lists are way too long. In this system primary care would be abundant. And I and many others have only horror stories of how big hospital systems, insurers and big pharma treat them badly. They would much rather have an empowered PCP on their side.
The only concern about primary care for patients is if the PCP is incented to not refer them to needed specialty care. In my system there would be no global capitation or risk to the PCP, and thus no incentive not to refer out. But no reason to refer out unnecessarily. They would do the right thing because it is the right thing. (It has taken Jeff Goldsmith 30 years to convince me of this). So there would be no need for insurance companies to manage primary care at all. No claims, no bills, no utilization management. Instead we should have 600,000 primary care docs paid well and able to manage their practices to do the right thing.
And this would probably involve a ton of variation. There would be PCPs who work in groups. There would be solo. There would be those specializing in specific types of patients (think kids or people with serious diseases or geriatricians). They would all make the same amount of salary but their practice’s revenue and number of patients would be adjusted in a similar way to how we do risk adjustment for Medicare Advantage now, but without the games, and with no profit motive.
This system would create a lot of innovation. PCPs would be responsible for those with chronic conditions. They would have budget from the $2,000 per head (of which they would get roughly $800 as income) to build remote monitoring programs, to use AI, to build teams of assistants and nurses et al.
So can it be done in the US? Yes it already has. I urge you to take the time to read this ingenious ChatGPT summary of the Nuka system in Alaska. (I believe created by Steve Schutzer MD). Nuka went from being a hidebound bureaucratic expensive system–that its patients hated–to being a system with culturally appropriate care that its “consumer-owners” love today. And its costs are lower and outcomes better. There are lots of other examples of similar approaches across the US. Just ask Dave Chase. They just haven’t scaled because the current incumbents have killed them. (One great example is this case in Texas where a hospital chain bought and killed a big primary care group led by Scott Conard because it was costing them $100m a year in reduced hospital FFS admissions).
What we need is to set up the incentives, prod doctors and patients hard to get into these arrangements and let American ingenuity and medical professionalism go at it.
The other side of the equation is the need to reign in the costs of specialty and hospital care. How this would happen is up for debate.
Continue reading…Avasure: Tech for helpful watching & remote care in hospitals
Lisbeth Votruba, the Chief Clinical Officer and Dana Peco, the AVP of Clinical Informatics from Avasure came on THCB to explain how their AI enabled surveillance system improves the care team experience in hospitals and health care facilities. Their technology enables remote nurses and clinical staff to monitor patients, and manage their care in a tight virtual nursing relationship with the staff at the facility, and also deliver remote specialty consults. They showed their tools and services which are now present in thousands of facilities and are helping with the nursing shortage. A demo and great discussion about how technology is improving the quality of care and the staff experience–Matthew Holt
Lynn Rapsilber on Nurse Practitioners
There are a lot of nurse practitioners in the US–over 400,000 (compared to around 900,000 MDs & DOs), and we are training 40,000 a year. But how they are going to be used is not entirely clear. Lynn Rapsilber is an NP whose organization, the National Nurse Practitioner Entrepreneur Network, is working to help her fellow NPs with their professional and business development. She came on THCB to discuss how NPs are developing and how she thinks NPs will contribute in the future as we deal with the current crisis in primary care–Matthew Holt
TytoCare–The Last Few Inches of Telehealth?
Tamir Gottfried, the Chief Commercial and Strategy Officer at TytoCare came on THCB to show us how their remote device works to deliver the last few inches of telehealth. Most telehealth is just a video call but with Tyto’s device, the patient can asynchronously (and/or synchronously) take their vital signs including videos and pictures of the skin, ears, mouth, heartbeat et al, and share it with their doctor. It actually amazes me that they haven’t been more popular but in the last few years Tyto has made significant inroads with health plans and providers delivering their devices, as well as adding chronic care management module, with a forthcoming smart clinic (AI) companion. Tamir explained who, how what and why to me, and gave a not too gruesome demo–Matthew Holt
Penguin–The Flightless Bird of Health AI
Fawad Butt and Missy Krasner started a new AI company which is building a big platform for both plans and providers in health care. Penguin Ai has a cute name, but is serious about trying to provide an underlying platform that is going enable agents across the enterprise. They are health care only, as opposed to the big LLMs. But does health care need a separate AI company? Are the big LLMs going to give up health? And what about that Epic company? Join us as we discuss how this AI thing is going to be deployed across health care, and how Penguin is going to play. Oh and they raised $30m series A to start getting it done–Matthew Holt
Boulder Care: Stephanie Strong & Marianna Zaslavsky
Stephanie Strong, CEO & Marianna Zaslavsky, the (relatively new) Head of Growth at Boulder Care came on THCB to tell Matthew Holt about their service which delivers medication assisted treatment for those suffering from substance used disorder, via telehealth. Stephanie has been one of the leading advocates for getting patients, especially those on Medicaid, access to treatment. She led a campaign to get the DEA to continue to allow substance abuse treatment using medication via telehealth. Marianna joined this summer with the goal of helping patients get access via managed care plans. We discussed a lot about the potential for Boulder to continue its harm reduction strategy for patients, and also the potential limits that might be coming via Medicaid reductions as part of the BBB. Stephanie & Boulder are supporting a campaign called Majority for Medicaid which is raising awareness about the impact of Medicaid cuts on these patients. Some of those stories are here
You can also text MAJORITY to 50409 to urge your representative to protect the promise of Medicaid.
Labcorp, Blue Shield and my $34.95 co pay (part 5)
By MATTHEW HOLT
I have been on a quest to try to understand why I am being charged $34.95 by Labcorp for some lab tests that I think should be free under the ACA preventative care statutes, and for which my insurer Blue Shield of Californian has issued me an EOB with a $0 co-pay.
It’s been a microcosm of the chaos of American health care so far, If you want to catch up here’s part 1, part 2, part 3 and part 4
You may recall that I had paid a $50 co pay for the lab tests connected to my preventative annual wellness visit in 2024 (and I didn’t pay attention) but that when I got a $34.94 charge from Labcorp in 2025 and found that Blue Shield said my copay was $0, I decided to investigate.
I have had a lot of help from Rhea, a senior customer service rep at Labcorp who I think is having nearly as much fun with this as I am. She told me that the co-pay Labcorp tries to collect is the lower of $50 or whatever the total bill is. For the 5 tests I had, Labcorp’s agreed rate with Brown and Toland Physicians (the Blue Shield-owned IPA that contracts with their HMO, of which I am a member) was $34.94. So that is the answer as to that charge.
But it still doesnt answer a couple more questions.
- Why was a subsequent lab test I had as a follow up also shown by Blue Shield as a $0 copay on the EOB?
- Why weren’t the lab tests I had considered preventative under the ACA and therefore also free?
Rhea’s guess for the first answer is that Labcorp receives a capitated amount for lab tests from Blue Shield or Brown and Toland, and that the second test was somehow covered under that. Maybe, but then why wasn’t the first one?
The second question takes me further down a rabbit hole. Rhea dug out the order from One Medical to Labcorp. You can see below that the CPT codes are on it (what the tests actually are) and also what the related diagnosis codes are.
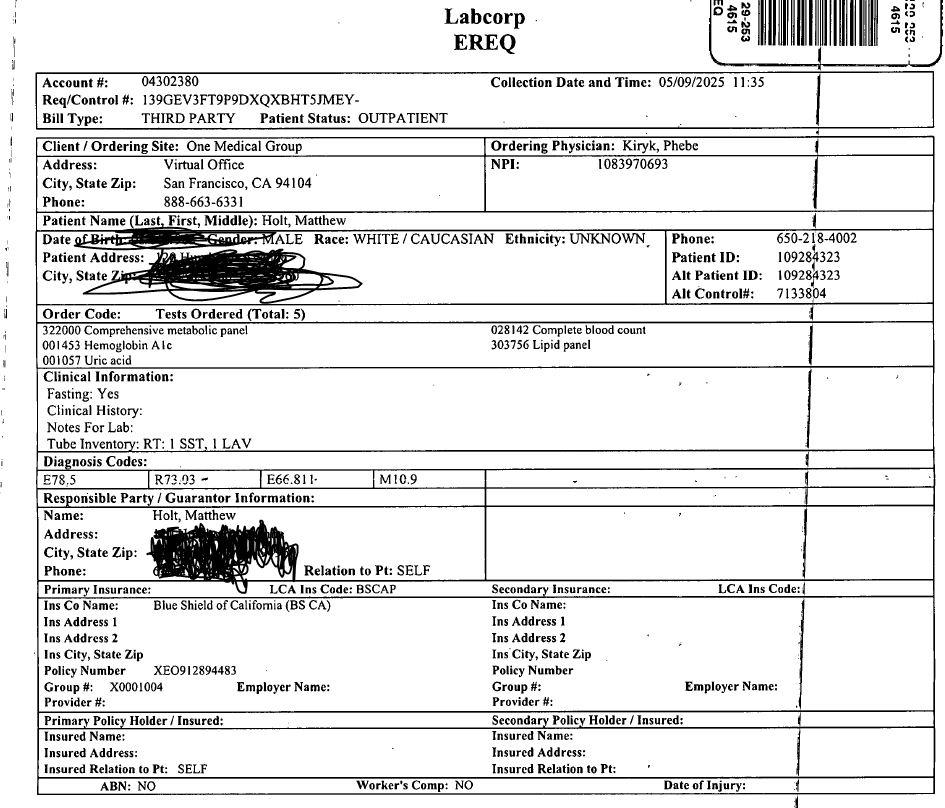
I of course asked chatGPT what those diagnosis codes were and the answer is
E78.5 = Hyperlipidemia (i.e. high cholesterol)
R73.03 = PreDiabetes
E66.811 = Obesity class 1
M10.9 = Gout
As you might suspect as a pretty typical 60+ year old American, I fit the bill for all those diagnoses. The CPT codes for the tests I had are complete blood count, Metabolic Panel, Hemoglobin (A1C), Lipid Panel, and Uric Acid (which causes gout).
Presumably all of those, with the possible exception of the Gout/Uric Acid, could be seen to be preventative. After all the CMS web site explains that preventative screening is free for “Annual Wellness Visits and Physical Exams, for instance with a primary care doctor and Health Screenings for blood pressure, cholesterol, blood sugar for diabetes, and various cancer screenings such as colonoscopies and mammograms”.
So why is this not free to me? Rhea from Labcorp suggests that Blue Shield initially issued me a $0 copay EOB but later should have reprocessed that when it got the bill from Labcorp, and told me to pay the $39.94. She also found that in addition to CMS suggesting what should be called preventative, Blue Shield of CA has a very long document with what it thinks is preventative care. You can see and download it here.
I asked ChatGPT to read it for me and after a bit of looking around we (that’s me and ChatGPT) concluded that E78.5 is in the list of applicable ICD-10 diagnoses codes for Annual health appraisal visits, which are a (free) covered service. So my high cholesterol should be screened for free.
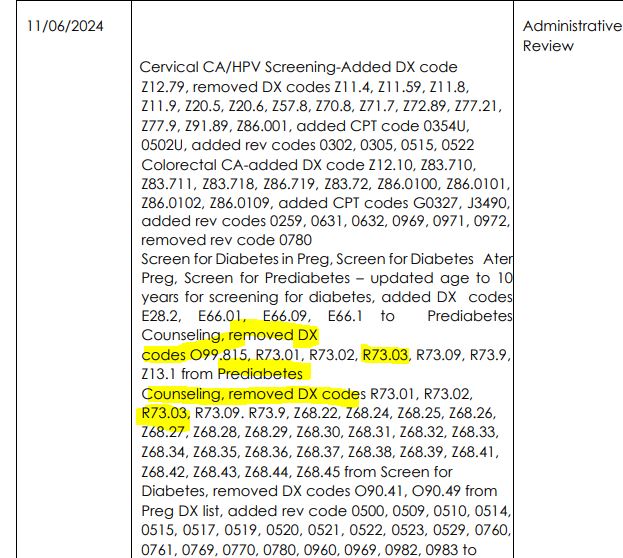
On the other hand there’s a whole section on Page 28 of the document discussing pre-diabetes education but it doesn’t explicitly say that an A1C test is covered under the annual wellness visit. And if you go way down, to page 116, there’s a table that suggests that last year a Blue Shield review removed several of the diabetes codes, including R73.03.
Now I am not going to pretend that I understand what the hell is going on in this document, and why (or whether) Blue Shield is able to change what CMS says it should do–if that is what in fact is happening. But it does seem weird.
And again, because there are no actual costs per test from Labcorp (there are charges per test but they are bundled and discounted on the bill), it’s impossible to tell what the contracted cost for each test was, and therefore whether I got some for free (as I think I should have) and what I was actually charged for.
Finally, I got very excited as Blue Shield sent me a message tonight which had an attachment which I think is a response to the grievance that was somehow filed for me by someone from their executive offices in part 2. But the attachment wasn’t properly formatted. So I don’t know what it says!
No less than I’d expect on this adventure.
But hopefully we are close to finding out who is charging whom for what and why!
UPDATE. I called Blue Shield’s grievance line and a nice customer service rep read me the letter that I couldn’t see online. Essentially Blue Shield has asked Brown and Toland to explain what happened. That grievance will take another 30 days! The rep wasn’t able to send it to me in my portal, but she could send me an email (It will be one of those secured ones that are super annoying to open). She told me it was sent while she was on the phone but 30 mins later, it’s not here!
Matthew Holt is the founder and publisher of THCB
Dr Kaelee Brockway on AI for physical therapy training
Dr Kaelee Brockway is a professor of education and physical therapy who has built a series of AI based “patients” for her PT students to train on. Kaelee is a pioneer in using these tools for training. She showed me the personas that she has built with LLMs that are now being used by her students to figure out how to train their soft skills–a huge part of any training. This a great demo and discussion about how clinical professionals are going to use LLMs in their training and their work–Matthew Holt









