By MATTHEW HOLT
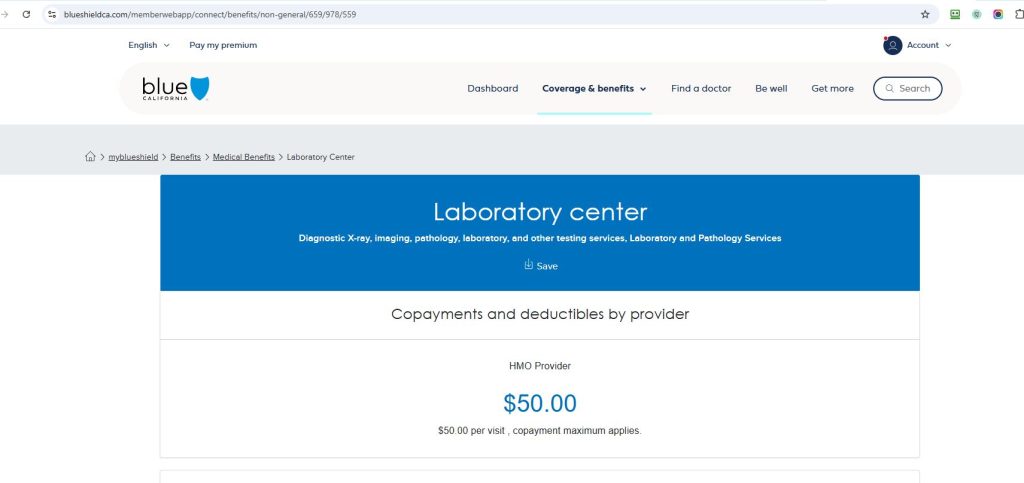
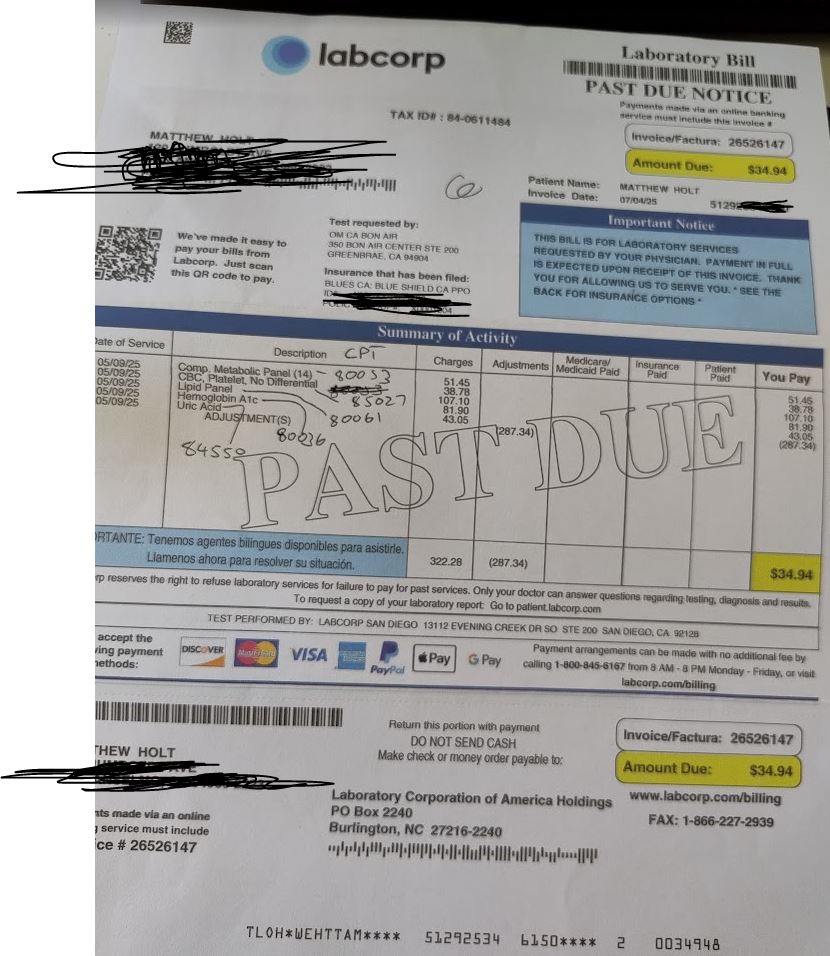
To join in the fun I am having with Blue Shield of California & Brown & Toland Physicians IPA being unable to tell me why I have a $34.94 bill for lab work (see image) that should either be covered as preventable under the ACA, or have co-pay of $50 (see image of the BS of CA screenshot for the $50), I called Labcorp.
After 6 minutes I got a very confused person. BTW there is NO way to communicate with Labcorp on the website, and if you put your invoice number into their IVR system there is NO way to get a human. The only way to do that is to hang up and start again, NOT put in your invoice number and hit 0. Then wait on hold with muzak to get a human. They then ask your DOB and phone number. The call center is in the Philippines BTW.
I explained that I wanted information on which test was not covered under the ACA. Brown and Toland/Blue Shield’s EOB says I have a $0 co-pay (see image).

The Labcorp rep told me that of the 5 tests done (with CPT code and price), 3 were not covered. The Lipid (85027 $107.10), the A1C (80061 – $81.90) Uric Acid (84550 $43.05). 2 of those 3 clearly are covered under the ACA. The Uric Acid one may not be according to my reading of the CMS site. Labcorp submitted that bill to Blue Shield. The rep consistently told me the claim was sent to Blue Cross Blue Shield of CA, which doesn’t exist.
At that point — 15 minutes in — the call dropped. I don’t know if they just hung up but they had asked for my phone number. They didn’t call me back.
But I am a pain in the ass, and I called them back. After roughly 4 mins on hold, I got another rep. She told me ALL of the CPT codes/lab tests were subject to copay. She told me that Blue Shield (NOT Brown & Toland Physicians) has bundled all of these codes and there is a co pay for all of them. Which is what the bill says.
So the only thing I can do is to send an email with the screenshot of the EOB, which is from the IPA not Blue Shield. So I did that and may get a response in 3-5 business days.
I know you are on tenterhooks. Let’s see what happens next but the complete absence of anything resembling consumer transparency or access to the relevant information makes a mockery of everything Paul Markovich says on stage.
UPDATE. Labcorp both emailed me back AND asked me to contact them on Linkedin. See what they asked for! Yes even though they have sent me a bill and I sent them the invoice number, they want every detail possible about the claim they ALREADY have!

Full email below just for giggles

Oh and when I went to DM them on Linkedin as they requested their account was not accepting DMs!
2nd UPDATE: A very nice man from the Blue Shield of California corporate office called me up. We discussed whether the care I got was preventative or not and why I was being charged the $34.94. Of course he didn’t know. He agreed with me that it was a shit show, and actually started to complain that sometime HE had been charged for preventative stuff he thought should have been free.. He didn’t have any solution other than calling Brown and Toland to cancel the charge, but I told him I didn’t want any special treatment (at least not yet!). I told him I wanted no special favors, but I wanted the claim reprocessed and an explanation.
And there’s a part 3!
Matthew Holt is the founder and publisher of THCB











